Medical Terms Used by Saints in Nauvoo and Winter Quarters, 1839–48
Douglas C. Heiner, Evan L. Ivie, and Teresa Lovell Whitehead
Douglas C. Heiner, Evan L. Ivie, and Teresa Lovell, “Medical Terms Used by Saints in Nauvoo and Winter Quarters, 1839-48,” Religious Educator 10, no. 3 (2009): 151–162.
Douglas C. Heiner (dcheiner@gmail.com) was a professor emeritus of pediatrics at the UCLA School of Medicine when this was written.
Evan L. Ivie (evanlivie@gmail.com) was director of the Joseph Smith Academy and BYU Semester at Nauvoo when this was written.
Teresa Lovell Whitehead (twhitehead@afwireless.com) was a winter 2004 student at the Joseph Smith Academy when this was written.
 Medical science was in its infancy during the Nauvoo and Winter Quarters period. Cause of infectious diseases were largely unknown. (Theodore Gorka, Emma Smith, the Elect Lady). Intellectual Reserve, Inc.
Medical science was in its infancy during the Nauvoo and Winter Quarters period. Cause of infectious diseases were largely unknown. (Theodore Gorka, Emma Smith, the Elect Lady). Intellectual Reserve, Inc.
A search of old documents, journals, and newspapers of the day will often mention but fail to clarify the medical terms used by Latter-day Saint pioneers. Consequently, we felt it important to gather as much data as we could and use modern medical terminology to clarify many original health-related records. We hope the information given below will be of interest to readers, particularly those whose ancestors had serious illnesses or died in Nauvoo or Winter Quarters in the years 1839 to 1848.
Medical science was in its infancy during the mid-nineteenth century. The terms people used to describe diseases then were different from those we would use today.[1] Causes of infectious diseases were largely unknown, and families described illnesses that caused death in the best way they knew how. Such diseases as measles, scarlet fever, and scurvy had telltale signs which generally permitted an accurate diagnosis. However, many reported causes of death such as “fever,” “inflammation,” “stone quarry death,” “winter fever,” “hyetic fever,” and so on could each have been used to describe a variety of diseases. Illnesses and causes of death were discussed with neighbors and sometimes with self-appointed “doctors” in the community. This provided a limited degree of commonality in describing major illnesses of the time but was often confusing.
Consider the setting in which the Saints lived. Few diagnostic facilities were available. There were no laboratories which could identify bacteria or viruses. X-rays, CAT scans, and MRIs were not known. Simple tests like blood counts, urinalyses, and blood chemistry determinations were not within reach. People frequently guessed what sickness they were dealing with. Even if they guessed correctly, there seldom was anything medical science could do to alter the course of the illness. Doctors sometimes did more harm than good with their prescriptions, purgatives, and blood-letting practices. Joseph Smith’s older brother Alvin was, in all likelihood, killed by the inappropriate administration of mercurous chloride (calomel) by a physician. After Alvin’s death, two consulting physicians who were surprised at Alvin’s demise performed a postmortem examination. They found that a concretion of calomel had blocked his small intestine, strongly suggesting that this blockage was the cause of his death.[2]
In April 1843, at a meeting with new immigrants, Joseph Smith said, “Doctors won’t tell you where to go to be well; they want to kill or cure you, to get your money. Calomel doctors will give you calomel to cure a sliver in the big toe. . . . And the lobelia doctors will do the same.”[3] It is heart-wrenching to think of oneself in the position of a Nauvoo Saint who had a serious illness to deal with.
We were able to find approximately one hundred perceived causes of death recorded by family members in newspapers and personal journals of the time and by sextons who were charged with keeping burial records for specific cemeteries. William Huntington, sexton for Old Nauvoo Cemetery, recorded many deaths. Families reported what they believed to be the cause of death of loved ones. This belief often was simply the most prominent symptom they had observed. The sexton, who was not a trained physician, recorded the family’s belief or his own interpretation of the cause of death.[4]
Though there are limitations in any assessment drawn from rather scanty data, we have utilized epidemiological information gleaned from the reported dates of death, ages of the people who died, recorded comments, and current knowledge of diseases to draw our conclusions. We have grouped certain symptoms together when we thought it appropriate. For example, malaria caused diverse symptoms, and malaria deaths were given various names. Other physicians may analyze recorded causes of death somewhat differently. Nevertheless, we have used our best judgment and in some instances have offered alternative possibilities. A more detailed discussion of deaths which occurred from 1839 through 1848—with an analysis of seasonal, gender, and age-related demographics—will be presented in a separate article.[5]
Comments Regarding Selected Causes of Death Recorded by Pioneers, 1839–48
Ague (Latin acuta, “sharp” or “acute”): Acute attacks of chills and fever. In the mid-nineteenth century, the term “ague” usually described malaria. Other terms such as “chill fever,” “recurrent chills,” or “bilious fever” also were descriptors of malaria. Malaria-related deaths usually occurred one to three months after a person had been bitten by a mosquito carrying virulent plasmodium parasites. The disease is commonly associated with marked malaise, a lack of energy, and a sense of depression. These three symptoms by themselves were commonly referred to as ague.
Apoplexy (Greek apopl?ssein, “to strike”): This refers to a stroke, often due to a hemorrhage or blood clot in an organ, usually the brain. It can cause various symptoms including weakness or palsy, altered sensation, and problems with vision, speech, or walking.
Bilious fever (Latin bilis, “bile”): Refers to fever associated with excessive bile or bilirubin in the blood stream and tissues, causing jaundice (a yellow color in the skin or sclera of the eye). The most common cause was malaria. Viral hepatitis and bacterial infections of the blood stream (sepsis) may have caused a few of the deaths reported as bilious fever.
Cancer (Latin cancer, “a crab”): Generally refers to a malignant tumor. Without surgery, radiotherapy, or chemotherapy, it usually spreads and causes death.
Canker (Latin cancer or cancrum, “a crab”): Refers to an ulceration, usually in the mouth. In the presence of malnutrition, debilitation, or immune deficiency, it may spread and cause tissue destruction, gangrene, and an agonizing death. Fortunately, the amount of pain experienced by patients with fatal canker is relatively small.In pioneer times the gangrene often turned tissues black, in which instance the disease was called “black canker.” Without antibiotics or adequate nutrition, progressive canker or cancrum oris was fatal in about 95 percent of cases, usually within one to three weeks of its recognition. Today this condition still occurs in countries where there is severe poverty and malnutrition.[6] Several diseases which weaken the immune system can add to the effects of malnutrition and debilitation, increasing the risk of progressive canker. These include measles,[7] gastroenteritis,[8] scurvy,[9] AIDS,[10] and, in the case of children, an initial or primary herpes virus infection in the mouth.[11] The beginning of the disease may look like simple aphthous stomatitis (common canker in the mouth). However, when it progressed into tissue necrosis or gangrene as a result of one or more of the above predisposing factors, the end result was usually the patient’s demise. Malaria, whooping cough, and severe diarrhea in all likelihood enhanced susceptibility in early Nauvoo and Winter Quarters. We have noted that the majority of fatalities caused by these diseases in Nauvoo coincided with the season of peak canker deaths. Indeed, any serious ongoing disease probably contributed to the risk of developing lethal canker in subjects with severe malnutrition. Canker deaths did, and still do, occur predominantly in young children.[12] The years of maximal susceptibility (ages one to seven) are years when the immune system is not yet fully mature and passive protection from mother’s breast milk is waning or has gone.
 Early cancrum oris; moderately advanced cancrum oris. 2009 Ansary-Custom Medical Stock Photo. All rights reserved.
Early cancrum oris; moderately advanced cancrum oris. 2009 Ansary-Custom Medical Stock Photo. All rights reserved.

Nowadays if the disease process is arrested through the administration of appropriate antibiotics and correction of malnutrition, the patient is left with debilitating scar tissue and disfiguration, often requiring heroic reconstructive plastic surgery.[13] Unfortunately the early Saints had no antibiotics and all too often did not obtain adequate nutrition.[14] They had little knowledge about what caused canker. Centuries ago, the condition was erroneously thought to be a cancer, hence the term cancrum. Later, in Great Britain, the commonly used terms were “mouth canker” and “noma.” Early Saints from England probably introduced the terms “canker” and “black canker” to other pioneers in describing this fatal condition. At present the four generally accepted medical terms for the condition are: cancrum oris, gangrenous stomatitis, necrotizing ulcerative stomatitis, and noma. Some authorities consider noma to be the preferred name.[15]
Early cancrum oris; moderately advanced cancrum oris
The disease usually begins on the gums inside the mouth, then progresses to spreading gangrene. It causes necrosis (death) of adjacent tissues, including bone and skin. If not treated by the administration of good nutrition and antibiotics, death ensues. One can see from the photos below that, if the disease is arrested, major reparative surgery may be needed.
Moderately advanced cancrum; advanced cancrum oris, arrested with nutrition and antibiotics
Cholera: A severe form of diarrhea caused by the bacterium Vibrio cholera. It results in massive loss of fluid into the bowel and severe watery stools. It can cause death from dehydration and shock within a few hours. It often occurs in epidemics. It is characterized by “rice water stools” and seldom has associated fever, colicky pain, or blood in the stools. If people of the mid-nineteenth century had known that giving boiled water containing appropriate amounts of salt and sugar by mouth at the onset of symptoms would counteract the dehydration, many lives could have been saved.[16]
Childbed fever or childbirth fever: Current medical terminology is puerperal fever or puerperal sepsis. It is a serious illness caused by bacteria entering the mother’s blood stream during the time of labor or delivery. It especially attends births in which there is poor or inadequate sanitation.
Colic (Greek kolikos, “pertaining to the colon”): Episodes of acute abdominal pain. There are numerous causes including gall bladder disease, gastroenteritis, food poisoning, cancer of the intestine, appendicitis, and so on. “Colic” was one of the many terms describing a symptom (in this instance pain) that was considered to be the cause of death.
Congestive fever: An abnormal accumulation of fluid or secretions in some part of the body, associated with fever. Deaths reported to be congestive fever probably were most often due to pneumonia.
Consumption (Latin consumptio, “process of consuming or wearing away”): This usually referred to tuberculosis. It described a chronic infection which slowly depleted the body reserves.
Cranium (Greek cranion, “skull”): When listed as a cause of death, it probably meant a blow to the head or a disease in the head such as meningitis, encephalitis, or brain tumor.
Croup (British dialect, “to cry or cough hoarsely”): Usually an inflammation of the larynx causing a typical croupy bark-like cough. It is most often caused by a respiratory virus, and occasionally the inflammation is so severe that it obstructs the intake of air, thus causing death. The danger of death is greatest in young children.
Dropsy (Greek hydropos, “of water”): An abnormal accumulation of fluid, especially in the lower legs and feet. Dropsy or edema in the legs may be secondary to malnutrition, weakness of the heart (heart failure), kidney disease, or old age. Occasionally, dropsy in other areas of the body were listed as causes of death: dropsy of the abdomen (ascites or fluid in the abdominal cavity), dropsy in the chest (usually due to weakness or failure of the left ventricle of the heart), or dropsy in the head (hydrocephalus).
 Edema or dropsy in the leg. Courtesy of Wikimedia.
Edema or dropsy in the leg. Courtesy of Wikimedia.
Dyspepsia (Greek dys + pepsis, “disturbed digestion”): Commonly associated with excessive production of hydrochloric acid causing inflammation of the stomach, lower esophagus, or duodenum, sometimes associated with peptic ulcers. Dyspepsia also may be associated with cancer of the stomach, intestine, pancreas, or esophagus.
Fits: Convulsions or sudden abnormal behavior.
Flux (Latin fluxus, “excessive flow”): A term frequently applied to diarrhea in adults.
Gropt (probably from French grippé, “seized”): A term frequently used to describe influenza.
Hooping cough or hoping cough (See pertussis)
Hyetic fever (Greek hyetos, “rain”): Fever associated with a period of rainfall.
Inflammation (Latin inflammare, “to set on fire”): Refers to redness, heat, and pain. It involves the accumulation in body tissue of white blood cells and chemical mediators of inflammation. It can occur in any part of the body. Sometimes only the term “inflammation” was provided as the cause of death.
Inflammation of the bowels: Diarrhea, dysentery, flux, colitis, or enteritis.
Inflammation of the brain: Meningitis, encephalitis, or brain abcess.
Inflammation of the head: Meningitis, encephalitis, brain abscess, or cellulitis (infection of the skin) of the scalp.
Inflammation of the lungs: Pneumonia or lung abscess.
Irraecepelas (Greek erythros + pela, “red skin”): The correct spelling is “erysipelas.” This refers to a spreading infection of the skin, usually due to streptococcus. If unchecked it may lead to sepsis (serious blood stream infection) and death.
 Erysipelas of the face. The darker areas are red and indicate the infected areas. Courtesy of Wikimedia.
Erysipelas of the face. The darker areas are red and indicate the infected areas. Courtesy of Wikimedia.
Erysipelas of the lower leg
Lung fever: Probably indicates pneumonia, lung abscess, or infection of the covering of the lungs (pleurisy).
Malaria (Italian mala + aria, “bad air”): A disease thought to be due to bad air in the mid-nineteenth century. It actually was caused by the bite of an anopheles mosquito transmitting plasmodium parasites which entered the victim’s red blood cells and destroyed many of them. There are four types of malaria parasites, Plasmodium falciparum being the one that is usually responsible for death. The disease is typically manifested by severe recurrent chills and fever, often with jaundice, sweating, and fatigue. Death, when it occurs, usually comes one to three months after exposure to mosquitoes carrying the parasite. Mosquitoes were prevalent mainly from July until the first frost in Nauvoo and Winter Quarters. Deaths attributed to ague were largely due to malaria in Nauvoo and Winter Quarters.
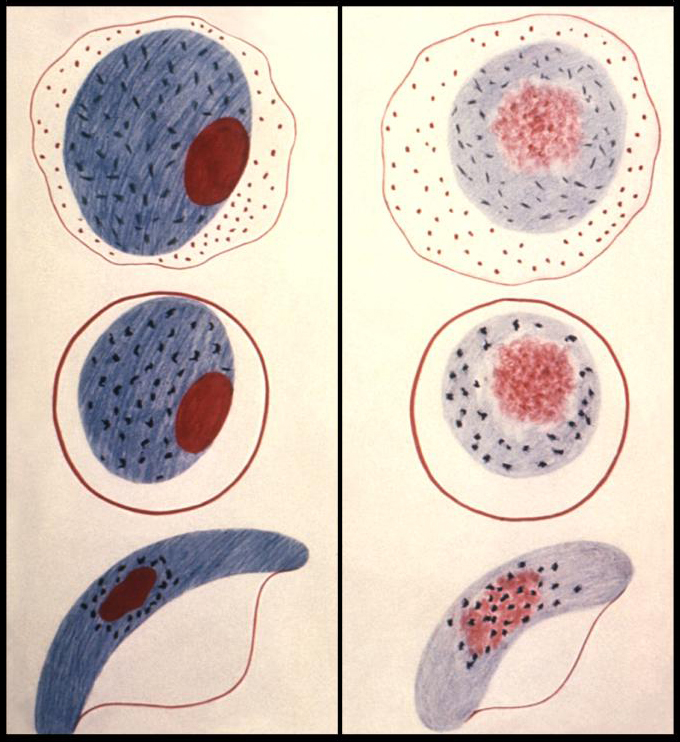 Mosquito-borne malaria parasites (left); normal and malaria-infected red blood cells (right). The four red blood cells marked "P" are infected with parasites. Courtesy of Centers for Disease Control and Prevention.
Mosquito-borne malaria parasites (left); normal and malaria-infected red blood cells (right). The four red blood cells marked "P" are infected with parasites. Courtesy of Centers for Disease Control and Prevention.
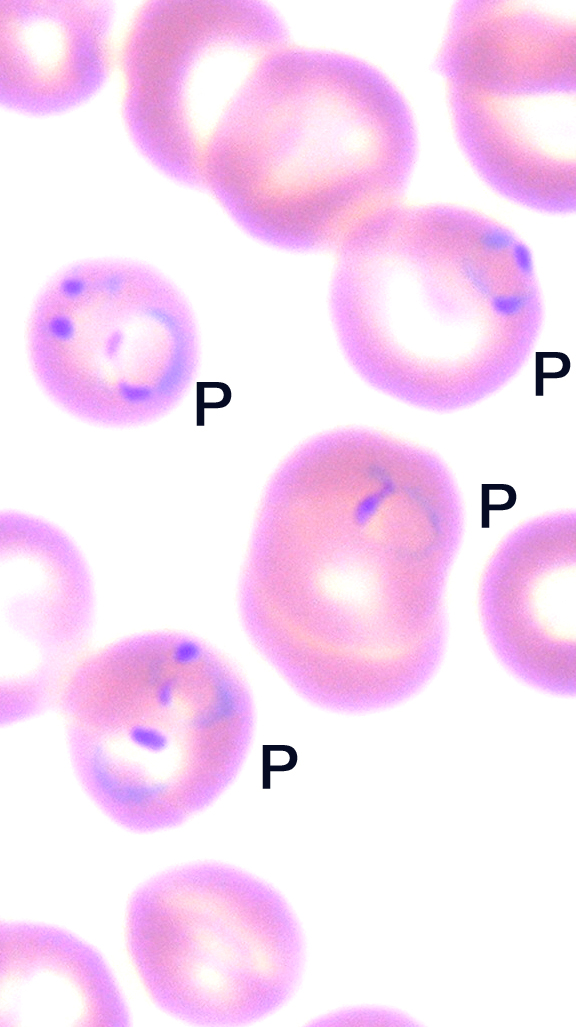 Mosquito-borne malaria parasites, normal and malaria-infected red blood cells
Mosquito-borne malaria parasites, normal and malaria-infected red blood cells
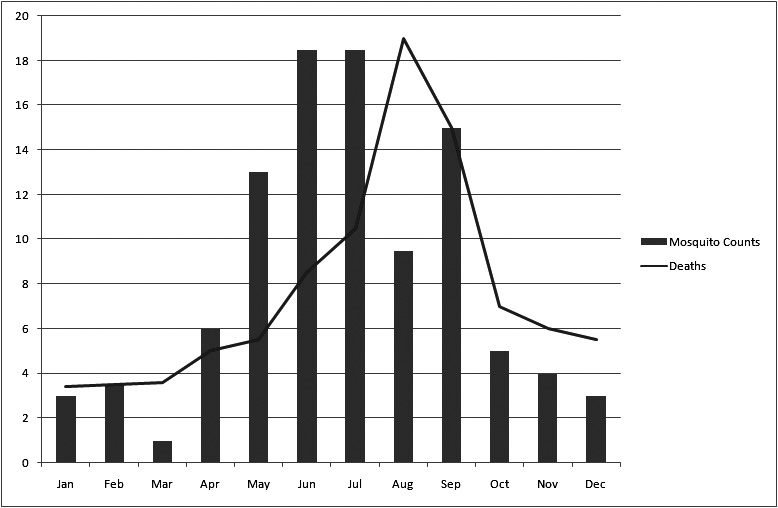 The above bars represent monthly mosquito counts obtained in an African community. The line indicates deaths due to malaria in the same community. Note that the greatest number of deaths occurred approximately two months after peak mosquito counts.
The above bars represent monthly mosquito counts obtained in an African community. The line indicates deaths due to malaria in the same community. Note that the greatest number of deaths occurred approximately two months after peak mosquito counts.
Mercurial diarrhea: This could refer to massive diarrhea of any cause, or it might refer to diarrhea initiated by the commonly prescribed calomel, a purgative prepared from the mercury compound mercurous chloride. If given in excess to a sick person, this laxative may cause or exacerbate diarrhea. If improperly diluted, it may cause blockage in the bowel. In either event calomel may contribute to or cause death.
Nervous fever (Latin nervosa, “composed of nerves”): It could refer to meningitis or encephalitis, or it could refer to a nervous reaction during a febrile disease such as malaria. Clues to its cause could sometimes be found in the time of year it occurred as well as in associated symptoms.
Noma (Latin nome, “corroding ulcer”): Spreading gangrene, nearly always beginning in the mouth but rarely in the nose or another part of the body. A synonym of canker, black canker, cancrum oris, and gangrenous stomatitis.
Numb palsy: A weakness, paralysis, or stroke associated with decreased sensation or numbness in part of the body.
Old age: It is of interest that this cause of death was listed for people ages 56 to 78. It probably was given as a cause of death when the family could not recognize any other specific cause.
Palsy (Latin paralysis, “loss of the ability to move part of the body”): Weakness or inability to move a part of the body.
Pertussis (Latin per + tussis, “extreme cough”): It is caused by the bacterium Bordetella pertussis. A whooping cough–like illness that is occasionally caused by B. parapertussis or by mycoplasmal or chlamydial organisms. In children, whooping cough often is associated with an inspiratory crowing sound or whoop, hence the name whooping cough. There may be some difficulty breathing at any age, but in infants and young children it may be so severe as to cause death.
Pleurisy (Greek pleuritis, “inflammation of the side or ribs”): The pleura is a covering on the surface of the lungs and the inner surfaces of the thoracic cavity. Pleurisy is often associated with pneumonia, but it can be caused without pneumonia by enteroviruses. It also may result from trauma to the chest wall.
Putrid sore throat (Latin putridus, “rotten”): This could have referred to diphtheria, peritonsillar abscess, or membranous pharyngitis due to either streptococcal infection or infectious mononucleosis. It also could have been associated with canker or black canker (cancrum oris) since this condition often results in foul-smelling breath.
Quinsy (Latin quinancia, “disease of the throat”): This usually refers to a peritonsillar abscess which can be acute and rapidly enlarging. It may cause death by obstructing the intake of air.
Remittent fever: Exacerbations and remissions of fever. It is most often due to malaria but could have other causes. Remittent fever of malaria may recur intermittently over a period of weeks or months. It may lead to death or may gradually subside due to the development of immunity.
Rickets: Deformity of the long bones in the legs or arms due to vitamin D deficiency. It can cause bowlegs, bumps where the cartilage and bones of the rib meet (rachitic rosary), deformities of the spine, and so on. It may occur in infants and young children who are exclusively breast fed and not exposed to sunlight for long periods of time. It is rather unusual for vitamin D–deficient rickets alone to be a cause of death. More unusual conditions such as renal rickets and vitamin D–resistant rickets may be fatal if not recognized and treated appropriately. Accurate diagnosis was often impossible in the mid-nineteenth century.
Rheumatic fever (Greek rheumatikos, “subject to a flow”): Sometimes called “traveling rheumatism” by early pioneers because it resulted in arthritis that migrated from joint to joint.[17] It is a complication of streptococcal sore throat or scarlet fever and may be associated with rheumatic heart disease (damage to the muscles and valves of the heart). Heart involvement was the usual cause of death.
Scurvy (S-curvy or corkscrew hairs): Scurvy results from vitamin C deficiency. Deaths from scurvy occurred most frequently in late winter and early spring before the fresh fruits, berries, and vegetables, which provide vitamin C, were on the family table. Corkscrew hairs arising from hair follicles which have pinpoint hemorrhages or petechiae are pathognomonic of scurvy. Scurvy causes bleeding in the skin and mucus membranes. It also causes spongy, bleeding gums and loose teeth. It is a known predisposing factor for canker or black canker.[18] When severe, scurvy can cause hemorrhage in the brain and death.
 Spongy necrotic gums in scurvy. This may predispose debilitated individuals to noma. Courtesy of Centers for Disease Control and Prevention.
Spongy necrotic gums in scurvy. This may predispose debilitated individuals to noma. Courtesy of Centers for Disease Control and Prevention.
S-curvy hair in scurvy, spongy necrotic gums in scurvy. This may predispose to noma in debilitated individuals
Spasm (Greek spasmos, “sudden involuntary muscle contraction”): Can be associated with convulsions or electrolyte disturbances.
Spinal irritation: Spine refers to the vertebral column. Spinal irritation was most commonly caused by meningitis, which usually led to death.
Stone quarry death: It could be due to an accident in the quarry, or it might refer to lung damage associated with inhaling large quantities of dust from stone cutting or polishing. Malaria also might have caused some deaths in quarry workers since the temple was located in a mosquito-infested area. Exposure to severe cold and dampness in wintertime could lead to death.
Teething: This refers to the appearance of teeth in young children. In itself, it almost never causes death. Rarely it may cause minor inflammation of the gums where a tooth is erupting. It was frequently listed as the cause of death when an underlying cause was not recognized.
Typhus fever (Greek typhos, “fever”): This is a disease caused by an organism called Rickettsia which is transmitted from person to person by the body louse, Pediculus humanus. It usually occurs during the winter months. Typhus fever was commonly confused with typhoid fever during the nineteenth century. Both diseases exhibit a high fever and a rash.
Typhoid fever: “Typhoid” means “typhus-like.” This disease is caused by the bacterium Salmonella typhi. It often involves infection of the bloodstream and may lead to infection in diverse parts of the body, especially the bones. Typhus fever does not cause bone infection or osteomyelitis, whereas typhoid fever does. It is now recognized that the osteomyelitis experienced by Joseph Smith in his youth was, in all likelihood, due to typhoid fever rather than to typhus fever as recorded by Joseph’s mother, Lucy Mack Smith.[19]
Ulcer (Latin ulcerous, “ulcer” or “sore”): Interrupted epithelial surface usually with an inflamed base. It generally refers to the gastrointestinal tract (stomach or duodenum), but it can occur in the mouth or on the body surface.
White swelling: This usually refers to swelling of the joints without redness or heat, as is often the cause with tuberculosis of the joints. We can only surmise that tuberculosis was the disease to which the Nauvoo sexton referred when he listed this as a cause of death.
Winter fever: This could be any fever leading to death during winter months. Most likely it refers to influenza or pneumonia, both of which were prevalent in the winter months.
Whooping cough (see pertussis).
Worm fever: Worms seldom cause fever and rarely cause death. In all likelihood, the involved person had a fever and a cause of death other than worms, but because worms were observed in the person’s stools, it was concluded that they caused the death.[20]
Notes
[1] For example, see Lyndon W. Cook, Nauvoo Deaths and Marriages (Orem, UT: Grandin, 1994); Fred E. Woods, “The Cemetery Records of William D. Huntington, Nauvoo Sexton,” Mormon Historical Studies 3, no. 1 (2003): 131–63; Veronica Christensen, Nauvoo Death Records—Records from Nauvoo Catholic Cemetery, Nauvoo Restoration, Inc, Nauvoo, IL 1996; Deaths and Burials in the Camp of Israel at Cutler’s Park and Winter Quarters beginning Sept. 1846. Data kindly provided by the Mormon Trail Center at Historic Winter Quarters, Omaha, Nebraska; Nauvoo period newspapers: Times and Seasons, Nauvoo Neighbor, and the Wasp.
[2] Scot Facer Proctor and Maurine Jensen Proctor, eds., History of Joseph Smith by His Mother (Salt Lake City: Deseret Book, 1996), 115–20.
[3] Joseph Smith, History of the Church of Jesus Christ of Latter-day Saints, ed. B. H. Roberts, 2nd ed. rev. (Salt lake City: Deseret Book, 1957), 5:357.
[4] George W. Givens, In Old Nauvoo: Everyday Life in the City of Joseph (Salt Lake City: Deseret Book, 1993), Chapter 10; George W. Givens, The Language of Mormon Pioneers (Springville, UT: Bonneville Books, 2003), 256.
[5] Evan L. Ivie, Douglas C. Heiner, Teresa Lovell, and Natalie Frietas, Causes of Death in Early Nauvoo and Winter Quarters, forthcoming.
[6] C. O. Enwonwu, “Noma: A Neglected Scourge of Children in Sub-Saharan Africa,” Bull World Health Organization 73, no. 4 (1995): 541–45; O. O. Denloye, G. A. Aderinokun, J. O. Lawoyin, and O. O. Bankole, “Reviewing Trends in the Incidence of Cancrum Oris in Ibadan, Nigeria,” West African Journal of Medicine 22, no. 1 (2003): 26–29.
[7] C. O. Enwonwu, W. A. Falkler, and E. O. Idigbe, “Oro-facial Gangrene (Noma/
[8] D. Lazarus, and D. A. Hudson, “Cancrum Oris—A 35-year Retrospective Study,” South African Medical Journal 87, no. 10 (1997): 1379–82.
[9] Lazarus and Hudson, “Cancrum Oris,” 1379–82.
[10] S. N. Ibeziako, D. E. Nwolisa, O. Nwaiwu, “Cancrum Oris and Acute Necrotizing Gingivitis Complicating HIV Infection in Children,” Annals of Tropical Paediatrics 23, no. 3 (2003): 225–26.
[11] Enwonwu, Falkler, and Idigbe, “Oro-facial Gangrene,” 159–71.
[12] K. W. Marck, “A History of Noma, the ‘Face of Poverty,’” Plastic and Reconstructive Surgery 111, no. 5 (2003): 1702–7.
[13] G. Thiery, O. Liard, and J. C. Duboscq, “Treatment of Noma [in French],” Médecine tropicale: revue du Corps de Santé colonial 62, no. 2 (2002): 193–8; D. Montandon and B. Pittet, “Lip Reconstruction in Noma Sequaelae [in French],” Annales de chirurgie plastique et esthétique 47, no. 5 (2002): 520–35.
[14] David R. Crockett, Saints in Exile (Tucson, AZ: LDS Gems Press, 1996), 307”; quote from Hosea Stout’s Journal.
[15] K. W. Marck, “Cancrum Oris and Noma: Some Etymological and Historical Remarks,” British Journal of Plastic Surgery 57, no. 6, (2003): 524–27.
[16] Lawrence M. Tierney, Stephen J. McPhee, and Maxine A Papadakis, Current Medical Diagnosis and Treatment (Norwalk, CT: Appleton and Lange, 1998), 1316.
[17] Givens, Language of Mormon Pioneers, 256.
[18] Lazarus and Hudson, “Cancrum Oris,” 1379–82.
[19] Proctor and Proctor, History of Joseph Smith, 71n5; see also 72–77.
[20] Text consulted with regard to selected infectious diseases: Red Book for PDA (Elk Grove Village, IL: American Academy of Pediatrics, 2003).
